Key points:
- A common degenerative joint disease of older people
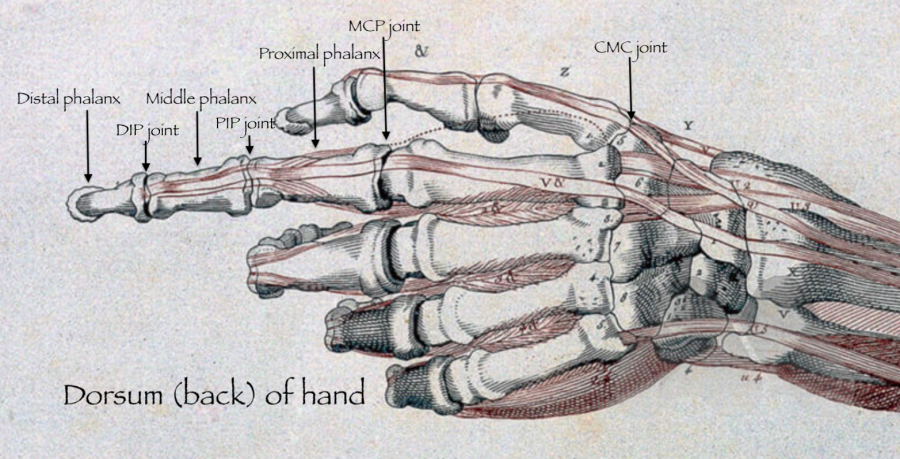
- Commonly affects the DIP joint, PIP joint, base of thumb (CMC joint)
- Hand therapy can be effective to help pain by using splints, education and strengthening and posture correction
- Many surgical options available to reliably relieve pain and improve function of the hand
What is it?
Arthritis can affect any joint in the body. The most common types of arthritis include osteoarthritis, rheumatoid arthritis and post-traumatic arthritis. Osteoarthritis is a degenerative joint disease where the smooth cartilage covering the bone ends, wear out, causing pain, swelling and stiffness and in the hand commonly affects the PIP joint, DIP joint and base of thumb (CMC joint). It commonly occurs in older people.
How do I know if I have osteoarthritis?
Common symptoms cause pain, and stiffness in the small joints of the hand. The knuckles can become swollen or show bumps and bony nodules called Heberden’s or Bouchard’s nodes in the fingers. Base of thumb arthritis can sometimes lead to the thumb being drawn into the palm and loss of a wide hand span. People often complain of difficulty opening jars and taps. X-Rays are often the most simple and effective way of showing arthritis.
What can I do about it?
There are no proven treatments to prevent or reverse arthritis. Treatment is aimed at managing pain, improving the function of the hand and in some cases improving the appearance of the hand.
Painkillers – Early symptoms of pain and swelling can be treated with simple painkillers such as paracetamol and anti-inflammatory medications.
Aids and modifications – Reducing the strain on your joints by using home modifications and aid appliances such as levers on taps, jar opening aids, either manual or electric devices can be found on the market and can help reduce pain.
Hand therapy – Hand therapists can provide simple strengthening exercises as well as correct any abnormal grip and pinch patterns that cause excessive strain on the joints. This can help in decreasing the load on supporting structures and cartilage.
Splints – Splints can be used to help support the affected area. These can be ready made and bought from a pharmacy and other outlets or can be custom made for you, from more rigid materials, by hand therapists.
Cortisone injections – Sometimes your doctor will recommend a cortisone injection to the joint to reduce the inflammation of the soft tissues that surrounds the joint. This can be effective for some people and can provide relief for many months to years in some situations. Repeated injections in a short space of time should be avoided.
Surgery – If these non-surgical methods fail to provide relief then surgery may be an option for more long lasting pain relief.
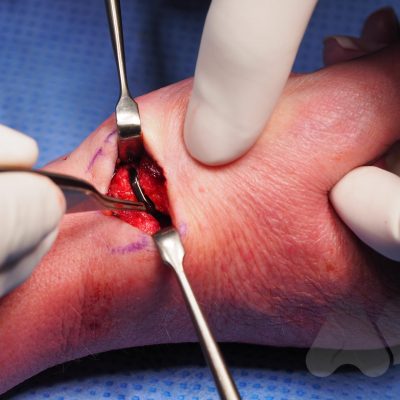
What types of surgery are available?
Depending on your main problem, different types of surgery may be appropriate. These include joint replacement, joint fusion or removing bones to create space in the joint.
Arthrodesis
This is the technique of fusing the joint in a position of best function that is appropriate to each individual patient. This is a very durable and reliable way of relieving pain and correcting severe deformity although it does prevent any movement of the affected joint from the fused position. It has been a technique employed since the early 1900’s with good long term results. It is particularly useful in younger patients with a requirement for heavy manual activity and commonly used to treat arthritis in the smaller joints of the fingers such as the DIP joints but can be performed in almost any joint. Risks of surgery include a failure to fuse the joint causing ongoing pain, risk of implant breakage or irritation to surrounding tissues, injury to surrounding structures including skin, nerves, blood vessels and cells that produce the nail and can also be complicated by infection.
Excisional arthroplasty and interposition
This is where a bone is removed to create space to unload the cartilage surface, to relieve pain and maintain movement. These techniques have been used since the 1950’s and 60’s in various joints in the hand.
Joint replacement
Joint replacements can use many types of materials including silicone, metal and plastic and pyrocarbon. Silicone joint replacements have been used in the small joints of the hand since the early 1960’s. They have a long track record and have a predictable outcome and ability to exchange implants if they fail. Modern day Metal on plastic implants have evolved since 1979 and now resemble modern day “mini knee replacements”. Pyrocarbon is a newer material and has been used since 2000. It can be implanted as a total joint replacement or hemiarthroplasty (replacing only one damaged side of the joint). Most joint replacement surgeries provide good relief of pain whilst maintaining motion however it is difficult to reliably improve range of motion in very stiff fingers.


Expected outcomes and risks of common treatments for finger arthritis?
To compare the outcomes of treatment we need to have a normal reference range against which to compare.
Normal motion in the PIPJ motion in older people is about 90 degrees. Normal grip strength in this age group is 22kg and pinch strength of 5kg.
PIPJ fusion fixes the joint in a position which is most functional. This differs for each of the fingers but does not allow for any movement from this position. It is very effective in relieving pain with average pain scores after the fusion heals of 0.4 out of 10. It allows for grip strength of 14kg and pinch strength of 3.9kg. It is very durable and in 95-98% of cases will last a minimum of 10yrs.
Silicone joint replacement of the PIPJ can on average provide a 50 degree arc of movement although this often depends on the starting range of movement prior to surgery. Pain is also reliably improved to 0.4 out of 10 and grip strength of 22kg and pinch strength of 4.4kg. 90% of silicone joint replacements will last a minimum of 10yrs.
Normal thumb movements are measured by a Kapandji score where normal movement is 10/10. Grip strength in average women of this age group is 22kg and in men 40kg and pinch strength in women 5kg and 8kg in men.
Thumb trapeziectomy restores thumb movement to 9.9/10 and relieves pain to 0.6/10. Grip strength on average is 25.7kg and pinch strength 3.6kg. It provides a durable solution with 97% of cases not requiring any further surgery after 10yrs.
Specific risks of trapeziectomy include thumb metacarpal migration causing weakness in grip strength and pain.
Thumb CMC fusion limits thumb movement to 5/10 on average. It is effective at relieving pain to 0.4/10 and maintaining grip strength to 23kg and pinch strength of 5.9kg. In 88% of patients who have had a CMC fusion, no further basal thumb surgery is required within 10 years.
Specific risks of CMC fusion include irritation or prominence of the metalware used to fix the joint or non-union at the surgery site.
Pyrocarbon joint replacement can maintain thumb range of movement to 10/10. It is an effective treatment option in relieving pain to an average of 0.6/10 and maintaining grip strength of 23kg and pinch strength of 6.4kg. Early results show that in 96.8% of cases, no further surgery is required within 5 years.
Specific risks of pyrocarbon joint replacement include ongoing pain and implant dislocation.